Ian Collins | 26 November 2023
Vaccine technologies have continued to improve greatly in recent years. However, vaccines are little use if people refuse to use them. Here we look at the precarious position of measles, a well-known but little-understood serious condition, which is held in check in most countries only because of high vaccine uptake.
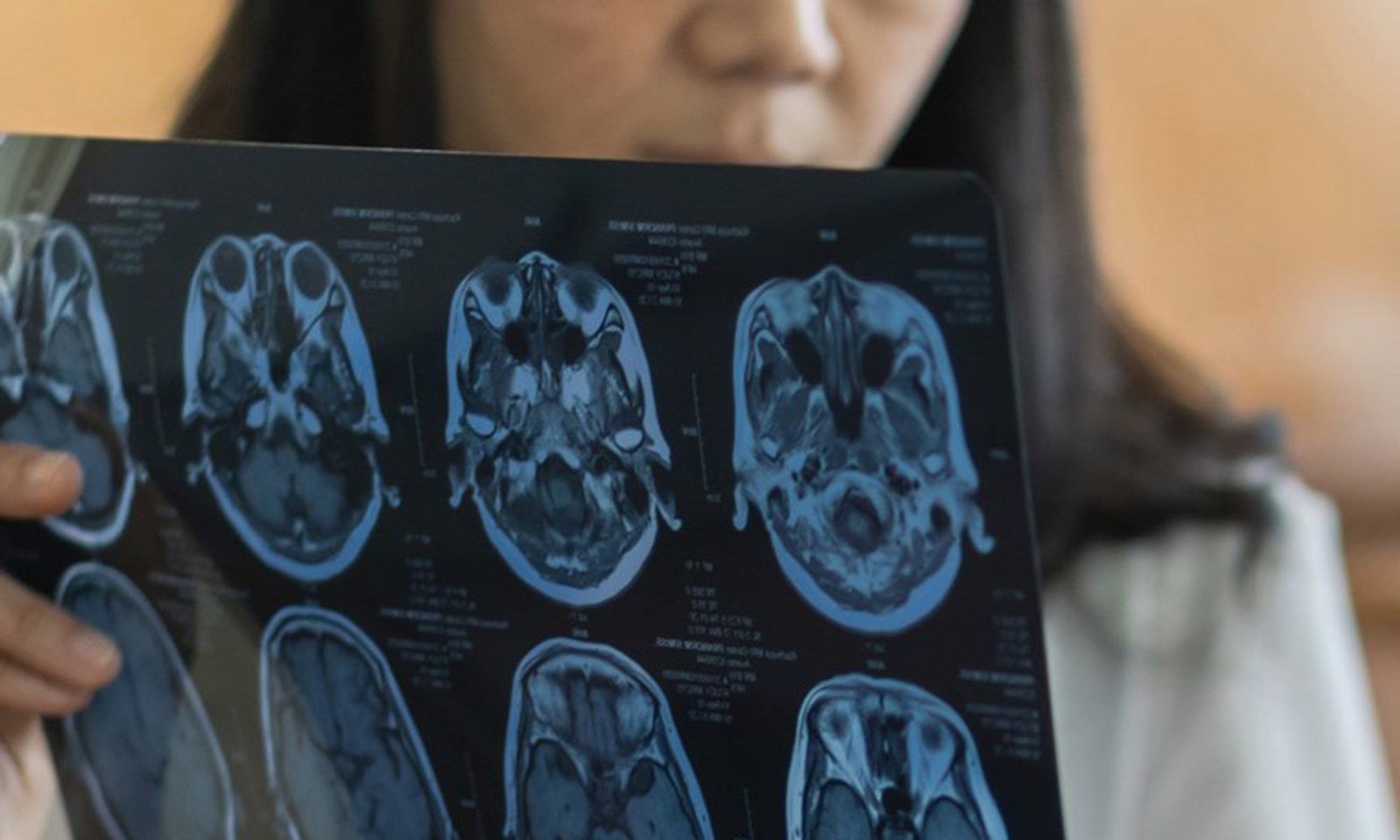
Measles remains one of the most contagious diseases known to science. Its potentially disastrous consequences, including meningitis, blindness and pneumonia, have generally been forgotten since high rates of vaccination have greatly reduced cases in many wealthier nations. However, the COVID-19 pandemic has accelerated trends in people who are sceptical of the efficacy and value of vaccines, including the MMR vaccine, which protects children against measles, mumps and rubella.
A recent poll found that 23% of Americans feel it is probably or definitely true that the MMR vaccine has been proven to cause autism, even though this finding has been widely discredited. 20% of those surveyed said they believed more people had been killed by COVID-19 vaccines than by COVID-19 itself.1
Rates of vaccination required to achieve herd immunity for measles are exceptionally high, likely around 95% due to the highly contagious nature of the disease. A report from the UK government highlights the increasing risk of a resurgence of the disease associated with low vaccine uptake. The risk is greater in areas with lower uptake. In the UK context, uptake in London is unusually low: only 74% of children have received the recommended two doses of MMR by age 5.2
In 2021 there were only 2 cases of measles in the UK. This rose to 54 in 2022. However, don’t be fooled by the small numbers. If the reproduction number rises above 1, then a tipping point could be reached. If an average case passes the disease to more than 1 other person, leading to exponential increases in the disease, a far larger outbreak could occur. The report concludes that London could see an outbreak of between 40,000 and 160,000 cases. Essentially continuing until the susceptible population has been exhausted by new infections. Estimated fatality rates range from 1 in 500 to 1 in 30003, although the report suggests 20-40% hospitalisation rates are expected. People who have been vaccinated usually have lifelong immunity.
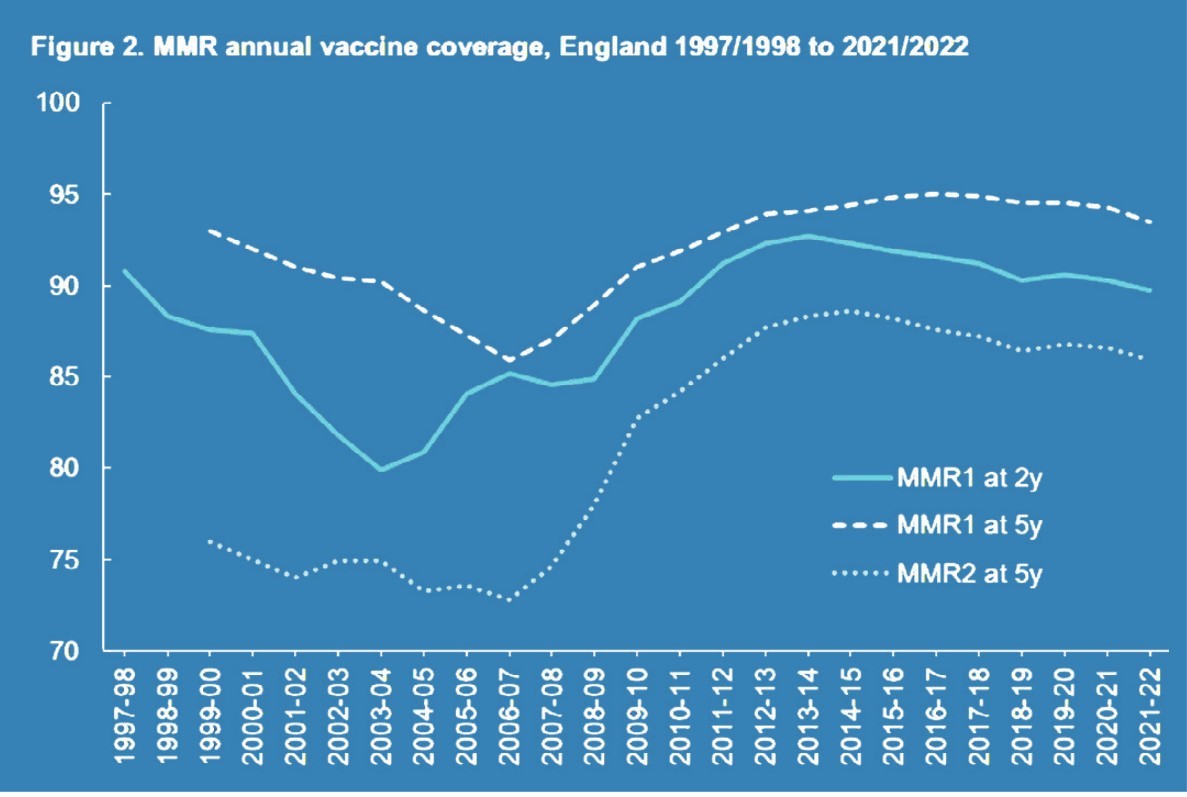
The recommendations include catching up on missed vaccinations for children and young adults. US vaccination rates overall are at 93%, a little higher than the UK, though in 9 states, plus the District of Columbia, rates are below 90%.4
The quick, safe, successful development of effective COVID-19 vaccinations was a triumph of science. However, some of the public health messaging surrounding their rollouts, and the wider pandemic response, may have had unintended effects including growing suspicion of recommendations emanating from national and multi-national organisations. Measles vaccination rates vary substantially, from 99% in some countries to below 50% in others.5
Even in countries with relatively high rates, we should remember those who reject vaccines are not distributed evenly throughout the population. Within any population, some groups will be at higher risk due to lower vaccine uptake. Any group of people likely to come into contact with one another, where material numbers are unprotected, is at risk of an outbreak – something that could be easily prevented using widely available vaccines.
References
- KFF Health Misinformation Tracking Poll Pilot | KFF.
- Risk assessment for measles resurgence in the UK | publishing.service.gov.uk
- Expert reaction to UKHSA risk assessment for measles resurgence in the UK, reporting that London is at risk of measles outbreaks | Science Media Centre
- Childhood vaccination rates drop dangerously low - The Washington Post
- Measles immunization rate by country, around the world | TheGlobalEconomy.com
Pacific Life Re Limited (No. 825110) is registered in England and Wales and has its registered office at Tower Bridge House, St Katharine’s Way, London, E1W 1BA. Pacific Life Re Limited is authorised and regulated by the Financial Conduct Authority and Prudential Regulatory Authority in the United Kingdom (Reference Number 202620). The material contained in this booklet is for information purposes only. Pacific Life Re gives no assurance as to the completeness or accuracy of such material and accepts no responsibility for loss occasioned to any person acting or refraining from acting on the basis of such material.
©2024 Pacific Life Re Limited. All rights reserved.

Ian Collins
VP, Medical Analytics










.png)
.png)















.png)